Vladislav Stoyanov
Email: vlady_vs@abv.bg
© 2019 Sift Desk Journals. All Rights Reserved
VOLUME: 3 ISSUE: 2
Page No: 160-167
Vladislav Stoyanov
Email: vlady_vs@abv.bg
Svetlana Bezhanova1, Vladislav Stoyanov2
1Department of gastroenterology, Medical Institute – Ministry of Interior, Sofia
2Department of general, abdominal and vascular surgery, Medical Institute – Ministry of Interior, Sofia
Svetlana Bezhanova, Vladislav Stoyanov, CHALLENGES IN THE DIAGNOSIS AND TREATMENT OF PATIENTS WITH COLORECTAL CANCER AND COVID-19 COINFECTION - CASE REPORT (2021) Journal of Anesthesia & Surgery 3(2) :160-167
Patients with colorectal cancer (CRC) are more likely to become infected with COVID-19 than healthy individuals. The risk of comlications and death in COVID-19 positive colorectal cancer patients is higher due to treatments that suppress the immune system.
We discuss a 71-year-old woman with a history of metastatic rectal cancer and underwent surgery and chemotherapy. With no clinical feathers of an acute abdomen or COVID-19 infection. Further researches are needed to rule out if COVID-19 can mask clinical and biological features presentation in cancer patients.
Keywords: metastatic colorectal cancer, COVID-19 infection, surgical treatment
On March 12, 2020, SARS-CoV2 (Corona Virus) or COVID-19 infection was declared a pandemic by the World Health Organization [1]. SARS-CoV-2 has been shown to cause acute respiratory distress syndrome (ARDS) with airborne transmission. The alternative way of infection is thought to be faecal-oral due to the presence of ACE-2 SARS-CoV-2 receptors in the gastrointestinal tract and the establishment of viral RNA in saliva and faeces [2, 3, 4, 5].
According to data available in the world literature, PCR tests for COVID-19 were performed in patients with pneumonia from faecal samples in which viral RNA was detected. In a study by Wang W et al. (2020), fecal PCR tests showed viral presence in about 30% of patients [6]. The virus can be detected in the feces for a longer time compared to the nasopharynx and saliva, by Zhang J et al., (2020). The authors think that asymptomatic COVID-19 positive patients can be diagnosed by this test [5].
The observed gastrointestinal damage from COVID-19 was small vessel thrombosis and non-occlusive mesenteric ischemia. Bhayana R et al. (2020) believe that the causes of intestinal ischemia are many and varied, but also emphasize the role of COVID-19 in thrombus formation in small blood vessels, including the intestinal wall. Typical intestinal ischemia, thrombosis in small blood vessels and necrotized intestinal wall ("dead bowel") have been observed in operated patients [7].
Cancer patients are considered the most vulnerable group in the current pandemic with COVID-19, due to their immunocompromised status from the neoplastic process and the ongoing chemotherapy or radiotherapy [8, 9]. Data from several studies in China and Italy show that mortality in such patients is about 6% and is higher than mortality in patients without established SARS Cov 2 - 2% [10,11]. The authors of two studies published data that patients with previous surgery and chemotherapy are at high risk for the development of severe infection, complications and death [12, 13].
Case report
We present a clinical case of a 71-year-old woman with metastatic colorectal cancer (CRC) known for about 2 years and polychemotherapy (PCT). The patient was referred for routine chemotransfusion for upcoming chemotherapy. The woman was with complaints of long-standing astheno-adynamia and once registered temperature 37.1ºС, without cough and runny nose, did not report the presence of abdominal pain, nausea or vomiting. From the physical status examination: woman of visible age around the actual, afebrile at the time of examination, pale skin and visible mucous membranes, mild abdominal pain, no evidence of peritoneal reaction and muscle defense, sluggish peristalsis. The laboratory tests shows anemic syndrome - hemoglobin level of 95 g/L and leukocytosis - 16.2 × 109/L, normal values of other blood parameters. COVID-19 tests were performed at the Emergency Medicine Department and negative serological test for SARS-CoV-2 antibodies (IgM and IgG) was detected. RT-PCR from nasopharyngeal secretion for COVID-19 was positive, established postoperatively.
Abdominal ultrasound found out the presence of circular heterogeneous fields on the anterior abdominal wall - parietal metastasis (Fig. 1); presence of pathological fluid in the abdomen - perihepatic (Fig. 2); dilated colon ascendens (Fig. 3) and colon transversum, pronounced aerocolia intralumenally (Fig. 4).
Presence of gas reverberations with impossibility to visualize large abdominal vessels - "vanishing vessels" phenomenon (Fig. 5); linear reflective, reverberating, hyperechogenic shadow of free gas in the right abdominal flank, between the right kidney and the liver (Fig. 6); bright point-shaped or star-shaped hyperechogenic foci with short distal reverberating hyperechogenic shadow - "comet tail" phenomenon leading to perforation of a hollow abdominal organ (Fig. 7).
The patient underwent abdominal and chest radiography, in which sickle-shaped shadows of free gas were found under the two diaphragmatic domes (Fig. 8) and hydro-aerial shadows, as well as the absence of typical pulmonary radiological data for COVID-19 (Fig. 9).
After consultation with a surgeon, the patient underwent emergency surgery and intraoperatively were found: tumor formation of the abdominal wall, measuring about 5 cm, which is extirpated firmly; presence of feculent peritonitis involving the right abdominal half, dilated caecum, ascending colon and transverse colon; perforation of the colon in the middle third of the ascending colon; secondary liver lesion about 0.5 cm in size, in the area of the fundus of the gallbladder; condition after anterior resection of the rectum with multiple retroperitoneal lymph nodes and fibrosis of the left colon (Fig. 10). A right hemicolectomy was performed, with an interruption of the intestinal passage about 20 cm from the ileocecal valve in a tight, and the proximal colon was interrupted at the middle-distal third border. We aspirated the faecal effluent and lavage was done. Ileo- and transverse stoma were done.
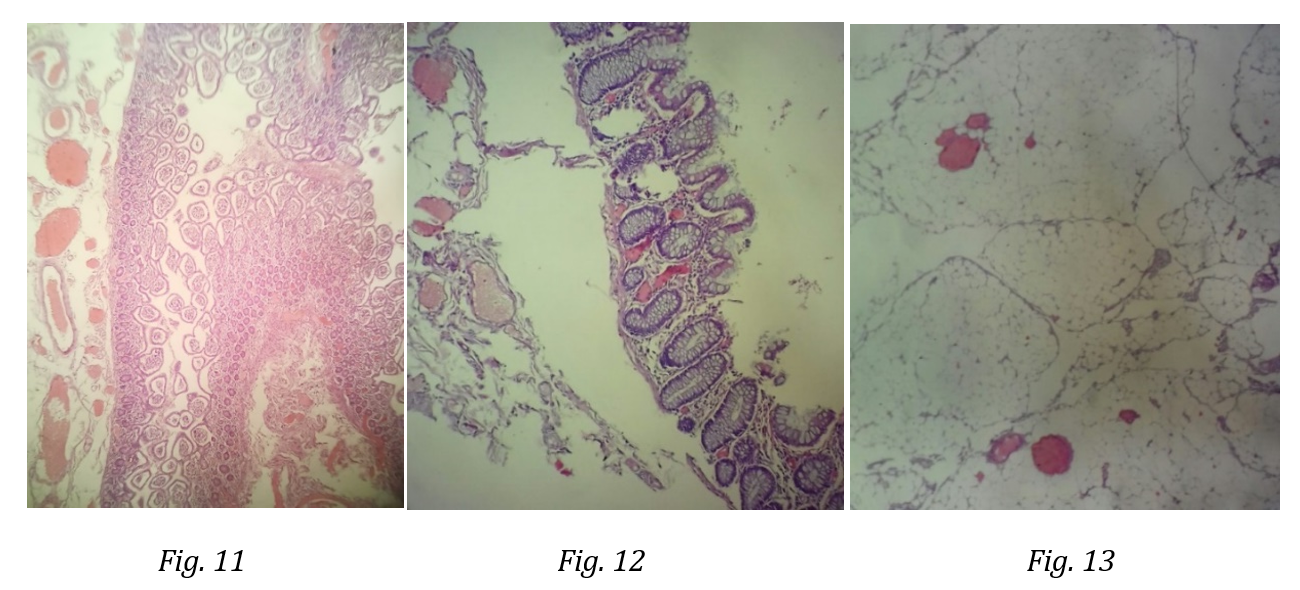
The data from the histological examination are for adenocarcinoma of the colon G2; metastasis of the abdominal wall from adenocarcinoma, fibrous tissue and focal inflammatory infiltrates with infiltration of pericolic adipose tissue; resection lines are without tumor infiltration; chronic inflammatory infiltrates mixed with leukocytes in the intestinal wall. Histological preparations with data for thickening of the vascular wall, vascular stasis, hyaline emboli and areas of necrosis (involvement of blood vessels in the mucosa, submucosal and adipose tissue) (Fig. 11, 12, 13).
On the second day after surgery, the RT-PCR test was positive and the patient was hospitalized in a specialized COVID-19 ward, where the lethal outcome occurred.
Despite the small number of publications and experience worldwide regarding emergency patients with CRC and COVID-19 infection, it is known that these are patients with a potentially high risk of developing postoperative complications, severe COVID-19 and death. The prognosis is likely to depend on the type and stage of the cancer. Highleyman L., (2020) believes that patients with metastatic cancer have a six-fold higher risk of severe complications than other cancer patients. COVID-19 positive patients and those receiving chemotherapy or radiotherapy are more at risk of developing acute respiratory distress syndrome, arrhythmias, shock, and acute renal failure [28].
According to Yang X. et al., (2020) mortality in patients infected with COVID-19 and colon cancer is about 6%, but is lower than in infected patients with diabetes (7%) and cardiovascular disease (11%) [29].
The case reported by us is of interest in several aspects: the patient has a history of previous surgery for metastatic rectal cancer (liver lesion, abdominal wall metastasis and peritoneal metastases); with several courses of PCT conducted in the previous months. There are no convincing clinical data for acute abdomen, but with instrumental data (ultrasound and radiological) for the presence of free gas in the abdomen. The patient was asymptomatic and with negative serology for SARS-CoV-2 infection, but with a positive COVID-19 PCR nasopharyngeal test, established postoperatively. Histologically adenocarcinoma was verified, ischemia of the intestinal wall and thrombi in the small blood vessels were found. Like Bhayana R et al., (2020) we believe that despite the many and varied causes of intestinal ischemia, the possible involvement of COVID-19 in thrombus formation in the small blood vessels of the intestinal wall and its presumed role of the virus for the more severe course of the disease and the poor prognosis. Possible co-infection with COVID-19 should be suspected in all surgical patients. This is essential in everyday clinical practice, on the one hand due to the higher risk of severe postoperative complications and death in such patients, on the other hand to protect medical teams from contamination [30].
Individuals over 60 years of age, immunosuppressed and comorbid are known to be more at risk of COVID-19 infection [14]. Of the COVID-19 studies, about 1% of positive patients had a history of previous or concomitant gastrointestinal cancer. Patients with SARS-CoV-2 infection and gastrointestinal malignancy have a higher risk of developing ARDS, respectively higher morbidity and mortality [15, 16]. According to the Italian Institute of Health (Istituto Superiore di Sanità, ISS) from 2003, 72 patients (20.3%) died of COVID-19 with a history of cancer in the last five years. Higher mortality was observed in males [17, 18, 19].
The mechanism by which the virus acts in cancer patients is still unclear [14]. In some patients with CRC, after infection with SARS-CoV-2, the virus may "wake up" to trigger an immune response with clinical symptoms. In about 1% of cases infected with SARS-CoV-2, patients are asymptomatic [20]. Urgent surgery is required in 1 / 4–1 / 3 of CRC patients [21-23].
Most often, these are elderly and immunosuppressed patients, with advanced tumors and after chemotherapy and radiotherapy [22]. COVID-19-positive asymptomatic patients operated on for CRC are thought to have a higher risk of postoperative complications and a higher risk of death [24,25,26,27].
Colon cancer remains a topical and socially significant problem due to the fact that it is the third leading cause of death and the fourth most common neoplasm [31]. Published data from a small number of studies to date indicate increased morbidity and mortality in patients with CRC and coinfection with COVID-19. In such patients, the therapeutic approach must be individual and complex.
Di Saverio S, Pata F, Gallo G, et al. Coronavirus pandemic and Colorectal surgery: practical advice based on the Italian experience [published online ahead of print, 2020 Mar 31]. Colorectal Dis. 2020;10.1111/codi.15056. doi:10.1111/codi.15056
Wan Y, Shang J, Graham R, Baric RS, Li F. Receptor recognition by novel coronavirus from Wuhan:An analysis based on decade-long structural studies of SARS. J Virol2020;JVI.00127-20.doi:10.1128/JVI.00127-20.
To KK, Tsang OT, Chik-Yan Yip C, et al. Consistent detection of 2019 novel coronavirus in saliva. Clin Infect Dis. 2020;ciaa149. doi:10.1093/cid/ciaa149
Young BE, Ong SWX, Kalimuddin S, et al. Epidemiologic Features and Clinical Course of Patients Infected With SARS-CoV-2 in Singapore [published online ahead of print, 2020 Mar 3]. JAMA.2020;e203204. doi:10.1001/jama.2020.3204
Zhang J, Wang S, Xue Y. Fecal specimen diagnosis 2019 novel coronavirus-infected pneumonia. J Med Virol. 2020;10.1002/jmv.25742. doi:10.1002/jmv.25742
Wang W, Xu Y, Gao R, Lu R, Han K, Wu G, et al. Detection of SARS-CoV-2 in Different Types of Clinical Specimens. Jama. 2020;29–30.
Rajesh Bhayana , Avik Som, Matthew D Li, Denston E Carey, Mark A Anderson, Michael A Blake, Onofrio Catalano, Michael S Gee, Peter F Hahn, Mukesh Harisinghani, Aoife Kilcoyne, Susanna I Lee, Amir Kasra Mojtahed, Pari V Pandharipande, Theodore T Pierce, David A Rosman, Sanjay Saini, Anthony E Samir, Joseph F Simeone, Debra A Gervais, George Velmahos, Joseph Misdraji, Avinash Kambadakone. Abdominal Imaging Findings in COVID-19: Preliminary Observations. Radiology, 2020; 201908 DOI: 10.1148/radiol.2020201908
Kamboj M and Sepkowitz KA: Nosocomial infections in patients with cancer. Lancet Oncol 10: 589 597, 2009.
Schrag D, Hershman DL and Basch E: Oncology practice during the COVID 19 pandemic. JAMA: Apr 13, 2020 (Epub ahead of print).
Onder G, Rezza G and Brusaferro S: Case fatality rate and characteristics of patients dying in relation to COVID 19 in Italy. JAMA: Mar 23, 2020 (Epub ahead of print).
Wu Z and McGoogan JM: characteristics of and important lessons from the coronavirus disease 2019 (COVID 19) outbreak in China: Summary of a report of 72,314 cases from the Chinese Center for Disease Control and Prevention. JAMA: Feb 24, 2020 (Epub ahead of print).
Liang W, Guan W, Chen R, Wang W, Li J, Xu K, Li C, Ai Q, Lu W, Liang H, et al: Cancer patients in SARS CoV 2 infection: A nationwide analysis in China. Lancet Oncol 21: 335 337, 2020.
Zhang L, Zhu F, Xie L, Wang C, Wang J, Chen R, Jia P, Guan HQ, Peng L, Chen Y, et al: Clinical characteristics of COVID 19 infected cancer patients: a retrospective case study in three hospitals within Wuhan, China. Ann Oncol: Mar 26, 2020 (Epub ahead of print)
Yu, J. et al. JAMA Oncol (2020) | Zheng, L. et al. Ann. Oncol. https:// doi.org/10.1016/j.annonc.2020.03.296 (2020) | Liang, W. et al. Lancet Oncol. 21, 335–337 (2020
View ArticlePellino G and Spinelli A: How COVID 19 outbreak is impacting colorectal cancer patients in Italy: a long shadow beyond infection. Dis Colon Rectum: Mar 17, 2020 (Epub ahead of print
Mao R, Liang J, Shen J, Ghosh S, Zhu LR, Yang H, Wu KC, Chen MH; Chinese Society of IBD, Chines Elite IBD Union; Chinese IBD Quality Care Evaluation Center Committee. Implications of COVID-19 for patients with pre-existing digestive diseases. Lancet Gastroenterol Hepatol. 2020 Mar 11. pii: S2468-1253(20)30076-5. doi: 10.1016/S2468-1253(20)30076-5.
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2018. CA Cancer J Clin. 2018;68(1):1–1.
Brenner H, Bouvier AM, Foschi R, Hackl M, Larsen IK, Lemmens V, et al. Progress in colorectal cancer survival in Europe from the late 1980s to the early 21st century: The EUROCARE study. Int J Cancer. 2012;131(7):7–7.
Istituto Superiore di Sanità. Report sulle caratteristiche dei pazienti deceduti positivi a COVID-2019 in Italia. Dati al 17 marzo 2020 (date accessed 19/03/2020)
View Article20. Ren Х , Chen В, Y Hong , Liu W, Qi Jiang, Jingying Yang, Qun Qian, Congqing Jiang. Challenges of CRC during COVID-19 epidemic Ann Transl Med 2020;8(7):498 |
View ArticleBaer C, Menon R, Bastawrous S, et al. Emergency presentations of colorectal cancer. Surg Clin N Am 2017;97:529-45.
Xu Z, Becerra AZ, Aquina CT, et al. Emergent colectomy is independently associated with decreased long-term overall survival in colon cancer patients. J Gastrointest Surg 2017;21:543-53
Zattoni D, Christoforidis D. How best to palliate and treat emergency conditions in geriatric patients with colorectal cancer. Eur J Surg Oncol 2020;46:369-78.
Spinelli A, Pellino G. COVID-19 pandemic: perspectives on an unfolding crisis. Br J Surg 2020 Mar 19 doi: 10.1002/bjs.11627. poor.
Segura-Sampedro JJ, Reyes ML, García-Granero A, de la Portilla F. Recomendaciones de actuación patología colorrectal de la AECP ante COVID-19 Documento 1_V1_marzo 2020 . org/images/site/slider/Recomendaciones_de_actuacion_ante_COVID.pdf (date accessed: 19/02/2020)
View ArticleQadan M, Hong TS, Tanabe KK, Ryan DP and Lillemoe KD: A multidisciplinary team approach for triage of elective cancer surgery at the Massachusetts General Hospital during the novel Coronavirus COVID 19 outbreak. Ann Surg: April 13, 2020 (Epub ahead of print).
Gallo G, Martellucci J, Sturiale A, et al. Consensus statement of the Italian society of colorectalsurgery (SICCR): management and treatment of hemorrhoidal disease. Tech Coloproctol.2020;24(2):145–164. doi:10.1007/s10151-020-02149-1
Liz Highleyman. Cancer Patients With COVID-19 May Have Higher Risk of Severe Illness and DeathCancer type, stage and treatment appear to affect the likelihood of poor outcomes.May 4, 2020
View ArticleYang X, Yu Y, Xu J, Shu H, Xia J, Liu H, Wu Y, Zhang L, Yu Z, Fang M, Yu T, Wang Y, Pan S, Zou X, Yuan S, Shang Y. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. 2020 May;8(5):475-481. doi: 10.1016/S2213-2600(20)30079-5. Epub 2020 Feb 24. Erratum in: Lancet Respir Med. 2020 Apr;8(4):e26. PMID: 32105632; PMCID: PMC7102538.
Simone В, E Chouillard1, S Di Saverio2, L Pagani3, M Sartelli, WL Biffl, F Coccolini6,A Pieri, M Khan, G Borzellino, FC Campanile, L Ansaloni, F Catena.Emergency surgery during the COVID-19 pandemic: what you need to know for practice Ann R Coll Surg Engl 2020; 102: 323–33 doi 10.1308/rcsann.2020.0097
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin [Internet].2018Nov1[cited2020 Apr 3];68(6):394–424. Available from:
View Article