Kasper Stokbro
Telephone(work): +45 65 41 34 75; Fax: +45 66 14 82 26
E-mail: kasper.stokbro@rsyd.dk
© 2019 Sift Desk Journals. All Rights Reserved
VOLUME: 3 ISSUE: 2
Page No: 153-159
Kasper Stokbro
Telephone(work): +45 65 41 34 75; Fax: +45 66 14 82 26
E-mail: kasper.stokbro@rsyd.dk
Rasmus Hartman-Ryhl, Marie Kjærgaard Larsen, Lillian Marcussen, Kasper Stokbro*
DDS, Department of Oral and Maxillofacial Surgery, Odense University Hospital, Denmark
Rasmus Hartman-Ryhl: OMF-resident; Marie Kjærgaard Larsen: OMF- resident;
Lillian Marcussen: PhD, Associated Professor; Kasper Stokbro: Consultant Surgeon
R.Hartman-Ryhl, M.K. Larsen, L.Marcussen, K.Stokbro, Transportation degrades the quality of plaster cast models in virtual surgical planning -Is it time for direct intraoral scanning? (2020) Journal of Anesthesia & Surgery 3(2) pp:153-159
The plaster cast model (PCM) needs to precisely reproduce the patient’s dentition to ensure optimal fit of the surgical splint; However, transporting physical models entails a risk of fracture of cusps, brackets or entire models. This study evaluated whether clinically significant differences (>1 mm) exist between the patient’s dentition and the PCM, and whether additional fractures occur from transportation from Odense, Denmark, to Rockhill, USA.
This prospective study enrolled 10 orthognathic surgical patients. Three digital models were produced per patient: A direct intraoral scan, a scan of the PCM in Odense, Denmark, and a scan of the PCM at 3D Systems, Rockhill, USA. Primary outcome was distance between 2 sets of digital models. Primary predictor was transportation.
The study found only 2 patients with no differences above 1 mm. Fractures occurred more often on brackets compared with teeth (Odds ratio: 5.4; P < .001). Fractures of brackets occurred twice as often on maxillary models (P = .045). Fractures occurred equally often during the 2 transportations.
In conclusion, surgical splints produced from PCM could incorporate inaccuracies primarily related to the orthodontic appliances. Therefore, it is recommended to minimize model transportation before digitization and preferably use intraoral scanning to minimize errors.
Key words: Orthognathic surgery, Surgical splints, dental models, digital occlusion, intraoral scanner, plaster cast model.
Plaster cast models (PCM) and intraoral scans (IOS) are considered accurate for clinical use and are used in a variety of dental clinical settings (e.g. fixed partial prosthesis, orthodontic treatment, etc.). Under ideal circumstances, both IOS and PCM produce equally precise results[1, 2, 7, 9–11]. However, the clinical reality presents with less than ideal circumstances and errors incorporated in the PCM could affect the precision of the orthognathic surgical outcome.
Physical PCM must be stored and transported to the nearest scanner to be digitized. During transportation parts of the PCM may be chipped off. Errors in the PCM could result in inaccurate fit of the surgical splint. This inaccuracy will increase the interdental distance or rotate the moving jaw-segment during intermaxillary positioning.
Both IOS and PCM show clinically acceptable results when used to produce occlusal splints for orthognathic surgery[12, 15]. The studies comparing precision between IOS and conventional PCM found that both methods have a margin of error of approximately 0.3 mm[1, 9, 10, 12, 15]. Therefore, this study uses a 1-mm margin between the digital models as both a clinical threshold, which could affect the fit of the surgical splint, and also to ensure that the differences does not originate from measurement errors.
This study aims to evaluate whether clinically significant differences (>1 mm) exist between the patient’s dentition (IOS) and the PCM, and whether additional clinically significant differences (> 1 mm) occur from transporting the PCM from Odense, Denmark, to Rockhill, USA. Clinically significant differences were interpreted as fractures and chippings of the PCM during transport. The null-hypothesis was that no difference exists between the digital models.
To test the hypothesis, the authors implemented a prospective observational study. The cohort was composed of 10 orthognathic surgical patients treated in the Department of Oral and Maxillofacial Surgery at Odense University Hospital from September 2017 to March 2018. Inclusion criteria were orthognathic surgery without segmented maxillary procedures. Exclusion criteria were if the PCM were damaged beyond clinical use during transport. All patients signed written consent forms to be included in the study before enrolment. This study did not influence the patients’ treatment, but included only a second scan of the patients’ PCM before sending these to 3D Systems (Rockhill, SC, USA). Intraoral scanning was also performed as per department standard to ensure accurate recordings of the patients’ dentition. No intervention was performed on the patients and therefore this study was exempt from ethical approval by the institutional review boards. All participants were treated in accordance with the World Medical Association Declaration of Helsinki (October 2000).
2.1. Variables
The primary outcome variable was the maximum distance between the IOS and the scan of the PCM. Secondary outcome variables were the number of contacts, which deviated by more than 1 mm between the direct and indirect scan and if these, were situated on the brackets or the dentition. Primary predictor variable was the difference between direct IOS and indirect scan of the PCM.
2.2. Study setup
Patients were initially treated with decompensatory orthodontic treatment before surgery. Upon completion of the pre-surgical orthodontic treatment, the position of the teeth was retained with passive orthodontics. Then, PCM of the dentition were made from alginate impressions by the orthodontists in private practice. Each model was wrapped in bubble wrap and sent by currier delivery service from the orthodontists to the Department of Oral and Maxillofacial Surgery, Odense University Hospital. The patients were evaluated clinically by an oral and maxillofacial surgeon and this included a cone beam computerized tomography scan (NewTom 3G, NewTom, Verona, Italy). The Department of Oral and Maxillofacial Surgery is implementing a fully digital workflow; therefore, the patients also underwent intraoral scanning using the Trios scanner (3-Shape, Copenhagen, Denmark). The PCM were also digitized using the Trios scanner at the Department of Oral and Maxillofacial Surgery (Odense, Denmark). The models were again wrapped in bubble wrap and sent to 3D Systems (Rockhill, SC, USA) for final digitization for the virtual surgical plan. Thereby, three digital models could be compared: The direct IOS (intraoral scanning with Trios scanner), the indirect scan (PCM digitized with Trios scanner) and the digitization performed by 3D Systems (PCM digitized at 3D Systems).
The three sets of digital models were prepared in MeshMixer (Autodesk Inc., San Rafael, CA, USA). The models were cut using the plane cut function in the middle of the orthodontic brackets. Additional sets of models were created to enable alignment of the different models, all were cut just above the orthodontic bracket to avoid errors in model registration. In 3D Slicer (version 4.10.0; www.slicer.org), the models were aligned using the surface registration function (Settings: RigidBody, Number of iterations: 2000, Number of landmarks: 200, Maximum distance: 0.1 mm). Following registration, the distance between the models was quantified using the model-to-model distance function and analysed using the ShapePopulationViewer (version 1.3.2; www.nitrc.org/projects/shapepopviewer) (Fig. 1).
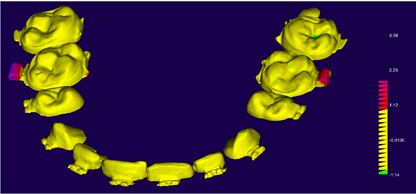
Fig 1. Surface to surface distance map measuring the distance between the intraoral scan and the digitized plaster cast model. Yellow areas indicate less than 1 mm between the digital models, red to purple indicates differences above 1 mm, which indicated fractures occurred between digitization of models. Green area indicates air trapped in alginate impression and filled with plaster during casting. All measurements are in mm.
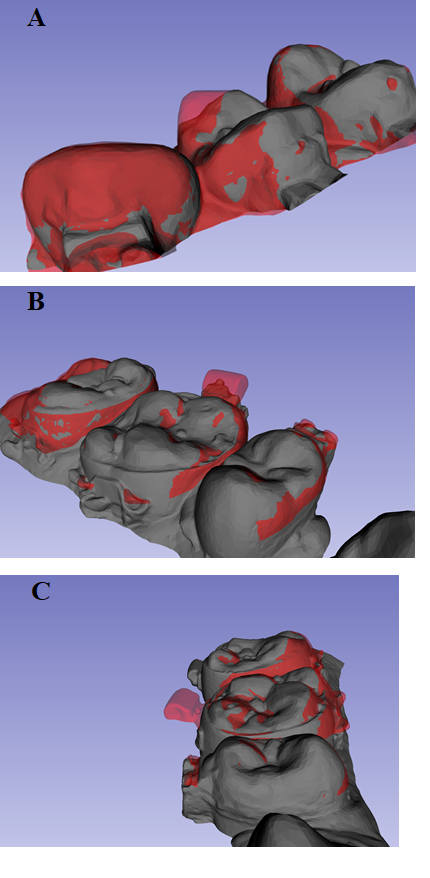
Fig 2. Visual inspection of differences between digital models evaluated as fractures in the plaster cast models during transport. (A) Fracture of a cusp, tooth 14, on plaster cast model after transportation of model from the Department of Oral and Maxillofacial Surgery, Odense, Denmark, to 3D Systems, Rockhill, USA. (B,C) Difference between intraoral scan and fractures of orthodontic appliance on the plaster cast model digitized by a Trios scanner at the department: (B) fracture of orthodontic appliance on tooth 16, (C) Fracture of orthodontic appliance on tooth 26.
2.3. Outcome measurements
The distance between the two models was calculated in relative distance. Positive measurements between the IOS and the PCM meant that the surface of the intraoral scan was further coronal to the PCM. Positive measurements between the indirect scan with Trios compared with the 3D scan performed at 3D Systems meant that the PCM was positioned coronal to the 3D Systems model. Positive measurements were interpreted as flaking or fractures of the PCM during transport (Fig. 2).
The largest distance was measured at both the dentition and at the orthodontic brackets for each model. Furthermore, the number of teeth and brackets with distances exceeding 1 mm were counted.
2.4. Statistics
Data was analysed using STATA 15.2 (STATA Corp Lt, College Station, TX, USA). The descriptive variables were analysed using Fisher’s exact test. Continuous variables were compared between groups by Wilcoxon sign-rank test. Comparing the number of differences larger than 1 mm between the teeth and the orthodontic brackets were compared using McNemar’s exact test to calculate odds-ratio and 95% confidence interval. The level of statistical significance was set at P ≤ 0.05. A clinically relevant difference was defined as more than 1 mm difference between digital models.
From the 10 consecutive patients included in the study, 1 patient was excluded because both models were damaged beyond repair during transport to 3D Systems. In 1 patient, the maxillary model was excluded, as a wrong model was scanned and the original model was sent to Medical Modelling without a Trios scan. Thus, the cohort included for analysis consisted of 17 models from 9 patients (Table 1). In this cohort, 6 patients had a model with at least 1 clinical difference above 1 mm when comparing the PCM with the IOS and 5 patients had at least 1 model with differences above 1 mm when comparing the PCM with 3DS. There was no significant difference in the amount of difference whether the models where transported from the orthodontist to the department or from the department to 3D Systems.
Table 1: Demographic description
|
|
IOS vs PCM |
PCM vs 3DS |
P-value |
|
Patients (N) |
9 |
9 |
|
|
Models (N) |
17 |
17 |
|
|
Clinical differences ( > 1 mm) (N) |
|
|
|
|
Patient |
6 (67%) |
5 (56%) |
1.00* |
|
Models |
8 (47%) |
8 (47%) |
1.00* |
|
Errors on teeth |
1 |
2 |
1.00* |
|
Errors on brackets |
8 |
7 |
.632* |
|
Maximum difference (mm) |
|
|
|
|
Teeth (median, range) |
.54 (.14–1.15) |
.50 (.10–2.06) |
.757$ |
|
Bracket (median, range) |
.99 (.23–3.38) |
.52 (.21–2.10) |
.158$ |
* Fishers exact test
$ Wilcoxon Rank-Sum test
Abbreviations: IOS, intraoral scanning, PCM, plater cast model digitized by a Trios scanner at the Department of Oral and Maxillofacial Surgery, Odense University hospital. 3DS, plater cast model digitized by 3D Systems, Rockhill, USA.
The locations of differences larger than 1 mm were primarily brackets (Table 2). Fractures occurred on the model’s brackets compared to cusps with an overall odds-ratio of 5.4 (P < .001). This showed, that the risk of a clinically significant difference on the brackets was much more likely than on the teeth. The sizes of the differences between digital models were also significantly larger for brackets compared to cusps (P = .002 & P = .015) (Table 3). Plotting the size of the difference between the digital models revealed that the brackets on the maxillary models were at a risk of large fractures (Fig. 3). The brackets on the maxillary models had twice as many clinically significant differences as the mandibular models, and the differences on the brackets were approximately twice the size (Table 4).
Table 2. Comparing the location of differences (>1 mm) between dentition or bracket.
|
Bracket
Cusp |
0 mm |
>1 mm |
Total |
|
0 mm |
431 |
38 |
469 |
|
>1 mm |
7 |
0 |
7 |
|
Total |
438 |
38 |
476 |
A: All comparisons between models
P = .000 (McNamar’s exact test)
Odds-ratio: 5.43 (95% CI: 2.39 – 14.41)
B: Intraoral scan compared with plaster cast models
|
Bracket Cusps |
0 mm |
>1 mm |
Total |
|
0 mm |
217 |
20 |
237 |
|
>1 mm |
1 |
0 |
1 |
|
Total |
218 |
20 |
238 |
P = .000 (McNamar’s exact test)
Odds-ratio: 20 (95% CI: 3.20 – 828.96)
C: Gypsum models vs. 3DS virtual models
|
Bracket Cusps |
0 mm |
>1 mm |
Total |
|
0 mm |
214 |
18 |
232 |
|
>1 mm |
6 |
0 |
6 |
|
Total |
220 |
18 |
238 |
P = .014 (McNamar’s exact test)
Odds-ratio: 3 (95% CI: 1.14 – 9.23)
Table 3. Measuring the distance between digital models by location on teeth or brackets
|
Median (Range) |
Teeth |
Brackets |
P-value |
|
IOS compared with PCM |
.54 (.14–1.15) |
.99 (.23–3.38) |
.002* |
|
PCM compared with 3DS |
.50 (.10–2.06) |
.52 (.21–2.10) |
.015* |
*Wilcoxon Sign-Rank test.
Abbreviations: IOS, intraoral scanning, PCM, plater cast model digitized by a Trios scanner at the Department of Oral and Maxillofacial Surgery, Odense University hospital. 3DS, plater cast model digitized by 3D Systems, Rockhill, USA.
Table 4. Comparing the number of differences above 1 mm between digital models evaluated by Maxilla or Mandibular location.
|
|
Mandibular models (N=18) |
Maxillary models (N=16) |
P-value |
|
Models with errors of more than 1 mm |
|
|
|
|
Teeth (N) |
1 |
2 |
.455* |
|
Brackets (N) |
5 |
10 |
.045* |
|
Maximum distance in model (Median (Range)) |
|
|
|
|
Teeth (mm) |
.55 (.10–2.06) |
.57 (.21–1.2) |
.849$ |
|
Brackets (mm) |
.64 (.23–1.69) |
1.31 (.21–3.38) |
.025$ |
* Fishers exact test
$ Rank sum test

Fig 3. Boxplot comparing the distance between digital models. Abbreviations: IOS, intraoral scanning, PCM, plater cast model digitized by a Trios scanner at the Department of Oral and Maxillofacial Surgery, Odense University hospital. 3DS, plater cast model digitized by 3D Systems, Rockhill, USA.
The PCM used to produce the surgical splint needs to precisely reproduce the patient’s dentition to ensure optimal fit of the surgical splint; However, the transport of the physical models entails risk of fractures on cusps, brackets or entire models. Currently, the model is cast from alginate impressions at the orthodontists, transported to the Department of Oral and Maxillofacial Surgery (Odense, Denmark) for inspection by the surgeons and then sent physically from Odense, Denmark, to 3D Systems (Rockhill, SC, USA) for digitisation. This study evaluated if there was a clinically significant difference between the digital models obtained by direct IOS and scan of the PCM during inspection at the department, and likewise, if there were clinically significant differences between the scan of the PCM at the department and the digital model used to fabricate the surgical splints. Clinically significant differences of more than 1 mm were interpreted as fractures of the models during transport.
This study found clinically significant differences between the digital models and thus rejected the null-hypothesis. Only 2 of the 9 included patients did not have any differences of more than 1 mm either between the IOS and the PCM or between the PCM digitized at the Department of Oral and Maxillofacial Surgery and the PCM digitized at 3D Systems. This supports the concern that the precision of the surgical splints produced from PCM could be compromised. Differences between IOS and PCM of more than 1 mm could result in decreased precision of the orthognathic surgery, and could potentially result in need for a second rectifying surgery if not corrected. The results also showed, that if the surgical splint does not fit, the maxillary brackets are most likely to be the source of error.
The reason for differences between the digital models was most likely caused by damage during transport, but alternative explanations may also have influenced the outcome. The maxillary brackets are most likely to chip of during transportation since the brackets are placed laterally. The lateral position of the brackets may make the brackets more susceptible to fractures in case the box with the models was traumatised during transport. The more medial position of the brackets in the mandibular model may protect against fractures, as the base of the models may be the first point of contact. Alternative, the differences between the IOS and the PCM from the orthodontist may also be caused by air trapped in the alginate impression during plaster casting. However, there still occurred differences between the digitization of the PCM performed at the department and at 3D Systems, therefore some damage occurs during transportation. Additional sources of potential errors were examined and ruled out by visual inspection of the digital models, such as errors in the stitching of the IOS, misalignment of models during registration, or changes of orthodontic brackets or bands between alginate impressions and IOS. None of these potential sources of errors were found in the digital models.
The authors found no study evaluating damage to PCM during transport in the pertinent literature, and to the best of our knowledge, this is the first study to report on the problems with transportation of physical models for virtual surgical planning. However, previous studies imply that IOS produce similar levels of accuracy and found that IOS had many advantages over conventional impressions. Using IOS minimize time consumption, patient discomfort and sources of error (such as air trapped in either the alginate impression or the plaster casting)[1, 2, 7, 9–11]. The digital models provided by IOS provides a more stable arch with more flexibility, which could result in more accurate outcomes[3–6, 8]. Additionally, there is no need for physical storage, the IOS can be augmented in case of missing information without the need to start over and the scan can be shared instantly around the globe without loss of information[13, 14]. The only potential source of error in IOS was the risk of saliva contamination, which should be assessed and addressed during the scanning procedure[3–6, 8]. However, this does not seem to influence the clinical outcome and studies comparing IOS with conventional scans found a similar level of precision of the surgical splints when tested clinically[15].
The study is limited by a small sample size, where the large number of fractures surprised the authors. Furthermore, the results may differ between countries and departments depending on several clinical factors, such as quality of the currier service, stability of the PCM, and distance needed to transport the models. Thus, the results from this study may not be directly transferable to other departments.
In summary, the results imply that minimizing the amount of transportation of the models before they are digitized is preferable and we would recommend using direct IOS to minimize the sources of error that affects the fit of the surgical splints. If the surgical splints are produced from digitization of PCM, we recommend designing a sufficient distance (1-2 mm) between the surgical splint and brackets to prevent errors from possible fractures on the models.
Funding: Kasper Stokbro received doctoral research grants from the University of Southern Denmark, the Region of Southern Denmark and the Department of Oral and Maxillofacial Surgery, Odense University Hospital.
Competing interests: None.
Ethical Approval: No intervention was performed on the patients and therefore this study was exempt from ethical approval by the institutional review boards.
Patient Consent: All patients signed written consent forms to be included in the study before enrolment.
Albdour EA, Shaheen E, Vranckx M, Mangano FG, Politis C, Jacobs R (2018) A novel in vivo method to evaluate trueness of digital impressions. BMC Oral Health 18:1-7 PMid:29970056
View Article PubMed/NCBIAragón MLC, Pontes LF, Bichara LM, Flores-Mir C, Normando D (2016) Validity and reliability of intraoral scanners compared to conventional gypsum models measurements: a systematic review. Eur J Orthod 38:429-34 PMid:27266879
View Article PubMed/NCBIBoeddinghaus M, Breloer ES, Rehmann P, Wöstmann B (2015) Accuracy of single-tooth restorations based on intraoral digital and conventional impressions in patients. Clin Oral Investig 19:2027-34 PMid:25693497
View Article PubMed/NCBICeyhan JA, Johnson GH, Lepe X, Phillips KM (2003) A clinical study comparing the three-dimensional accuracy of a working die generated from two dual-arch trays and a complete-arch custom tray. J Prosthet Dent 90:228-34 00237-3
View ArticleChen SY, Liang WM, Chen FN (2004) Factors affecting the accuracy of elastometric impression materials. J Dent 32:603-9 PMid:15476954
View Article PubMed/NCBIDeLong R, Knorr S, Anderson GC, Hodges J, Pintado MR (2007) Accuracy of contacts calculated from 3D images of occlusal surfaces. J Dent 35:528-34 PMid:17418474
View Article PubMed/NCBIEnder A, Attin T, Mehl A (2016) In vivo precision of conventional and digital methods of obtaining complete-arch dental impressions. J Prosthet Dent 115:313-20 PMid:26548890
View Article PubMed/NCBIEndo T, Finger WJ (2006) Dimensional accuracy of a new polyether impression material. Quintessence Int 37:47-51
Goracci C, Franchi L, Vichi A, Ferrari M (2016) Accuracy, reliability, and efficiency of intraoral scanners for full-arch impressions: a systematic review of the clinical evidence. Eur J Orthod 38:422-8 PMid:26487391
View Article PubMed/NCBIHaddadi Y, Bahrami G, Isidor F (2017) Evaluation of Operating Time and Patient Perception Using Conventional Impression Taking and Intraoral Scanning for Crown Manufacture: A Split-mouth, Randomized Clinical Study. Int J Prosthodont. doi: 10.11607/ijp.5405 PMid:29145527
View Article PubMed/NCBIMangano F, Gandolfi A, Luongo G, Logozzo S (2017) Intraoral scanners in dentistry: a review of the current literature. BMC Oral Health 17:149 PMid:29233132
View Article PubMed/NCBINilsson J, Richards RG, Thor A, Kamer L (2016) Virtual bite registration using intraoral digital scanning, CT and CBCT: In vitro evaluation of a new method and its implication for orthognathic surgery. J Craniomaxillofac Surg 44:1194-200 PMid:27423538
View Article PubMed/NCBIPatzelt SBM, Emmanouilidi A, Stampf S, Strub JR, Att W (2014) Accuracy of full-arch scans using intraoral scanners. Clin Oral Investig 18:1687-94 PMid:24240949
View Article PubMed/NCBIPatzelt SBM, Vonau S, Stampf S, Att W (2013) Assessing the feasibility and accuracy of digitizing edentulous jaws. J Am Dent Assoc 144:914-20 PMid:23904578
View Article PubMed/NCBIShaheen E, Sun Y, Jacobs R, Politis C (2017) Three-dimensional printed final occlusal splint for orthognathic surgery: design and validation. Int J Oral Maxillofac Surg 46:67-71 PMid:27815012
View Article PubMed/NCBIShaheen E, Sun Y, Jacobs R, Politis C (2017) Three-dimensional printed final occlusal splint for orthognathic surgery: design and validation. Int J Oral Maxillofac Surg. doi: 10.1016/j.ijom.2016.10.002 PMid:27815012
View Article PubMed/NCBI