Landry Wakheu Tchuenkam
Tel: +237 691528498
Email: landrytchuenkus@gmail.com
© 2019 Sift Desk Journals. All Rights Reserved
VOLUME: 3 ISSUE: 1
Page No: 124-131
Landry Wakheu Tchuenkam
Tel: +237 691528498
Email: landrytchuenkus@gmail.com
Axel SM Nwaha1, Theodore B Sala1, Landry W Tchuenkam2*, Gael Dongmo2, Biyouma M Derboise2, Angwafo Fru III3
1Urology unit, Department of Surgery, Douala Laquintinie Hospital, Douala, Cameroon
2 Faculty of Medicine and Biomedical Sciences, University of Yaounde I, Yaounde, Cameroon
3 Department of Surgery and Specialties, Faculty of Medicine and Biomedical Sciences, University of Yaoundé I, Yaounde, Cameroon
%c3%96mer Faruk %c3%9cnverdi(unverdiomer@gmail.com)
Landry Wakheu Tchuenkam, Successful perineum and scrotal reconstruction after Fournier gangrene using rotation of a medial thigh fasciocutaneous flap. Report of a case in low-resource settings and literature review(2019)SDRP Journal of Anesthesia & Surgery 3(1)
Background: Fournier's gangrene is a form of necrotizing fasciitis involving the perineal and scrotal region. It is characterized by rapid and extensive tissue destruction associated with signs of systemic toxicity. It's a real medical and surgical emergency. The diagnosis is essentially clinical and assisted by imaging in cases of atypical presentation. The urgent medical care associated with extensive surgical debridement helps to reduce the morbidity and mortality of this pathology with devastating consequences. Secondly the treatment will consist of tissue reconstruction when local and general conditions permit.
Case Presentation: the authors report the case of a 54-year-old black obese man, who is semi-Bantu ethnic group. He was transported to the emergency department of Douala Laquintinie Hospital (DLH) for painful swelling and offensive smell from bursa and perineal region for 4 days prior to admission. These symptoms were preceded by progressive peri-anal painful swelling unrelated to stool and fever. The diagnosis of Fournier's gangrene following anal abscess was made. The initial care consisted of intensive resuscitation with correction of hydroelectrolytic imbalance, broad spectra antibiotics and analgesics. The patient subsequently underwent major debridement in the operating room. The second stage of management consisted of a cutaneous reconstruction using a rotating fasciocutaneous flap taken bilaterally from each anteromedial aspect of the thighs.
Conclusion: Fournier's gangrene is a serious and life-threatening condition. It requires early diagnosis, adequate treatment without delay associating resuscitation measures and extensive debridement in the operating room. The second stage of management consists of tissue reconstruction using skin grafts or fasciocutaneous flaps most often.
Key words: Fournier's gangrene, fasciocutaneous flap, reconstruction
Necrotizing soft tissue infections are a general term that includes necrotizing forms of cellulitis, fasciitis and myositis clinically [1]. These infections could damage various points: the epidermis, dermis, subcutaneous tissues, fascia and muscles. Fournier's gangrene is a rapidly progressive necrotizing fasciitis involving soft tissues of the perineum and external genitalia[2]. This infection, like all other forms of necrotizing fasciitis, is clinically characterized by extensive and fulminant tissue destruction, signs of severe systemic toxicity and high mortality[3]; this mortality rate varies between 7.5 and 50% depending on the series [4,5].
The term Fournier is given to this form of fasciitis by a French dermatologist, Jean-Alfred Fournier in 1883[6]. This is most often a poly-microbial infection [1,5], the bacterial flora depends on the site of origin. The germs most frequently involved enterobacteria, anaerobes, staphylococcus, streptococcus or fungi. Although several cases of idiopathic infection have been described, the source of infection for etiology is identified in almost 95% of cases[7–9]. The source may be colorectal, genitourinary, cutaneous or traumatic [2]. Colorectal origin is most common with perianal abscesses, colorectal cancer, rectal instrumentation [10]. The urogenital origin is objectified in 17 to 87% of cases [8,11], urethral stricture, urethral instrumentation and indwelling catheterization represent the clinical situations found. The incidence of the pathology varies according to the literature; the usual age of patients varies between 30 and 60 years, although cases in infants have been described. It is an essentially a pathology found in male who is ten times more attacked than women [2]. Notwithstanding the source of the infection, several conditions or factors increase the risk of developing the disease; they are found in 52 to 88% of patients [3]. Situations that depress immunity such as diabetes, alcoholism, chronic kidney disease, glucocorticoid therapy, immunosuppressive therapy, malnutrition and neoplasia [3,12].
Fournier's gangrene is a diagnostic and therapeutic emergency. The clinical presentation varies depending on the stage of infection, comorbidities and the general condition of the patient. In the early stage, the main manifestations of the disease are: pain (79%), erythema (71%), swelling (81%) [13]; these symptoms sit in the perineal, scrotal, or even at the peri-anal region. At the later stage, the pain becomes throbbing, the fever is permanent, and the general state deteriorates. There are also signs of skin changes such as bubbles, subcutaneous emphysema, greyish appearance of the skin, foul odor and cutaneous necrosis. Laboratory exams are not a great help to diagnosis but are used to evaluate the impact of the pathology. The CT scan is the imaging examination of choice [5], it helps to define the limits of extension of the disease, and makes it possible to identify the underlying causes sometimes. It should not delay the implementation of the treatment.
The management of Fournier's gangrene is a medico-surgical emergency, it is done in two steps. The first is the acute phases. It consists of resuscitation measures, including electrolyte balance and antibiotic therapy. This is followed by rapid extensive surgical debridement. Once the infectious process is postoperatively controlled and the budding is adequate, the second phase or skin reconstruction step is undertaken. Fournier's gangrene is the most common cause of genital and perineal skin loss [2]. Several processes for recovering losses of substances are described [14]; such as: second-stage wound healing, tension sutures, skin grafts or skin flaps can be used.
We report here a case of Fournier gangrene in a 54-year-old patient following a peri-anal abscess. The reconstruction of the tissues was done using a fasciocutaneous and pedicled flap from the inner thighs. We then carried out a literature review under PubMed and Embase, the key words being "Gangrene, Fournier, necrotizing fasciitis". We reviewed the observational, analytic and clinical case studies published over the last 10 years from May 2008 to May 2018.
CASE PRESENTATION
This is the case of a 54-year-old black man, who is semi-Bantu ethnic group. He was transported to the emergency department of Douala Laquintinie Hospital (DLH) for painful swelling with an offensive scrotal smell. Seven days before admission, the patient complained of a peri-anal pain which became permanent and was not aggravated by stool. The evolution three days later was marked by increasing of the pain which became an excruciating disability associated with scrotal swelling in the context of fever and chills. The patient is a married man, heterosexual, he had no history of chronic pathologies, there was no history of abdominal or perineal surgery and there was no notion of rectal instrumentation.
On clinical evaluation the patient was conscious, cooperative and oriented. There was altered general state according to stage 4 WHO classification. The initial parameters were: a blood pressure of 125/78 mm hg associated with tachycardia (104 bpm), tachipnea (24 breaths/min), fever (39.4°C) and good oxygen saturation (97%). We observed a pallor with some signs of dehydration. At the loco regional examination of the genitalia, there was an erythematous scrotal and anterior perineal swelling; it did not involve the penis. The swelling was very painful and associated with areas of necrosis and offensive smell. There was crepitus on scrotal and perineal palpation. The anal region revealed a right peri-anal swelling about 3 cm in diameter: it was warm erythematous and painful with no apparent fistula. The rectal examination and the rest of the examination were not contributory.
For the biological investigations: the full blood count revealed anaemia with Haemoglobin at 6.9 g/dl, microcytic at 79 fl. There was leucocytosis at 12 x 106 / l, with granulocytic predominance. The rest of the biological examination, notably: blood sugar level, transaminases, serum electrolytes and renal function were within normal ranges.
At the end of the clinical examination, we diagnosed a Fournier’s gangrene complicating a peri-anal abscess. The initial management consisted in placing two intravenous lines for hyper hydration, analgesia, triple antibiotics (ceftriaxon, gentamycin and metronidazole) parenterally. Blood transfusion was done. The first unit of blood was transfused pre-operatively and the second unit per-operatively. The indication to urgent surgery was due to the presence of subcutaneous emphysema; also, no morphologic investigations were done. Six hours after admission, scrotal and perineal debridement was done associated with the drainage of an anal abscess under spinal anesthesia. During this initial intervention, the tissue seems inflated with areas of necrosis at the scrotum. Bubbles of air were produced having an offensive smell. Following the persistence of picks of fever at 40°C and pus from the perineal region, a second debridement was done 72 hours later. This permitted appropriate exploration of various zones of pus collection. The analysis of the pus collected per-operatively revealed Klebsiella oxytoca sensitive to 3rd generation cephalosporin.
We observed favorable results after the second post-operative debridement, pain regression was observed as from the second day. Antibiotherapy was done for 10 days and analgesia, gastric protectors, prevention of thromboembolic disease and sit baths administered three times daily. Following the absence of purulent perineal discharges, signs of wound healing in a clean perineal region (figure 1); tissue reconstruction was done in 46 days following initial debridement. We opted for a covering with a pedicled fasciocutaneous rotation flap taken off at the anteromedial sides of the thighs (Figure 2). The appearance of postoperative reconstruction is shown in Figure 3. Under local postoperative care, we had good flap holding with correct healing and a satisfactory aesthetic appearance.

Figure 1: Aspect of the scrotal and perineal area after debridement and local care
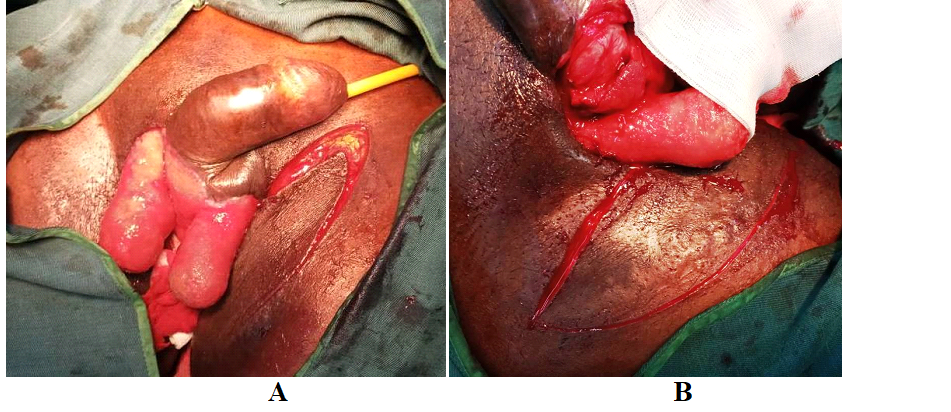
Figure 2: Intraoperative steps: mobilization of the medial fasciocutaneous
A: right side
B: left side

Figure 3: Post-operative appearance
The first descriptions of this pathology were made by Avicenna (1025) and Baurienne (1764) who described a rapidly extensive idiopathic gangrene of the perineal soft tissue. [15]. The name "Gangrène de Fournier" was attributed to pathology in 1883 by Jean-Alfred Fournier, a Parisian dermatologist. This is a true medical and surgical emergency. The diagnosis is essentially clinical, helped by imaging. It is based on the initial clinical finding of painful scrotal and perineal swelling in a patient with comorbidities[2]. In the evolutionary stage, the pain becomes permanent, throbbing, and atrocious; leading to insomnia associated with a patent clinical infectious syndrome and altered general state. The diagnosis, although difficult at the early stage, becomes obvious in the presence of area of necrosis, an offensive smell from the perineum and the presence of crepitus on palpation. [2,3]. Without management, the course of the disease lends to multiple organ damage and death.
Imaging is a tool to help diagnosis but does not constitute a barrier to starting treatment. Plain radiographs and ultrasonography of soft tissue can show the presence of air. The CT scan is the first intension imaging[5], it can be used in cases where the diagnosis is ambiguous with a high specificity compared to ultrasound and standard radiographs [16]. In case of necrotizing fasciitis, it can highlight tissue inflammation with thickening of fascia, gas, and abscess. It helps to define the limits of debridement and to identify possible etiologies[5,16].
Biological examinations are not very specific [1], abnormalities are leucocytosis, acidosis, coagulation disorders, elevation of creatinine, C-reactive protein, creatine kinase and transaminases. The elevation of the last two biological parameters is highly suggestive of fascial and muscle involvement, which is a factor of distinction with non-necrotizing infections. Several tools to help the diagnose of Fournier's gangrene have been evaluated. The LRINEC (Laboratory Risk Indicator for Necrotizing Fasciitis) score is the most used one [17]. Initially, this score was used to differentiate necrotizing fasciitis from other types of soft tissue infection. Subsequently, it proved to be also a good predictor of the severity of the disease[18]. This score is calculated from 6 biological parameters: creatinine, blood glucose, CRP, leukocyte count, hemoglobin, and natremia. This score makes it possible to classify patients in three categories: category 1 with a score ≤5 (low risk); category 2 with a score between 6 and 7 (intermediate risk); and category 3 with high risk, a score ≥8. The probability of the patient having necrotizing fasciitis is <50%, between 50 – 75% and > 75%, respectively. Our patient described above had a score of 8.
Evaluation of the severity of the pathology and the risk of death may be possible using this prognostic score [18]. A score ≥ 9 is associated with a probability of 93.7% of deaths.
Once the diagnosis is established, the care is urgent and without delay [19,20], the resuscitation will be aggressive, it will consist in an equilibration of the electrolyte imbalance, an initial broad spectrum antibiotherapy secondarily adapted to the results. Hyperbaric oxygen did not show a net benefit in the prognosis [19], resuscitation will be under close observation of the patient. The debridement should immediately follow the resuscitation as soon as the hemodynamic state of the patient is stabilized; it must be early (less than 24 hours) and the most complete possible [19]. When debridement is delayed, initially perineal gangrene extends rapidly to the anterior abdominal wall and posteriorly extends to the gluteal muscles [1]. Areas of necrosis are a poor reflection of the extent of subcutaneous tissue destruction. Therefore, the debridement must interest all the devitalized tissues, infiltrated by pus, gas and it will have to stop in healthy zone. Note that second-line debridement within 24 to 48 hours may be indicated postoperatively depending on the appearance of the lesions and the clinical condition of the patient [7]. Diversion colostomy and urine diversion or urethral catherisation may be undertaken to facilitate local postoperative care.
Fournier's gangrene is an extensive necrotizing fasciitis of the soft tissues of the perineum and external genitalia. This is the first cause of skin loss in the scrotal area [7]. The second stage of management involves soft tissue reconstruction. The good time for this reconstruction is not fixed. It varies according to the locoregional state of the wound. Obtaining an adequate tissue response to local care is a good marker for initiation of reconstruction [2]. This includes the presence of granulation tissue and cleanliness of the wound.
Several plastic reconstruction techniques are possible; the choice of surgical reconstruction depend on the area to be covered, the material available and the financial cost. These techniques have been the subject of several published articles [21]. Table 1 is a summary and comparative table of these different processes. There is no superior reconstruction technique to another. In addition to the characteristic of the skin defect, the elements to be taken into account in the choice of the reconstruction technique are multiple: the aesthetic appearance as well as the sensitivity of the skin obtained at the end, the number of surgical intervention required, the post-operative complications at the reconstruction area and donor site morbidity. When the loss of substance is localized to the scrotum and constitutes less than 50% of the scrotal surface, delayed primary closure, or scrotal advancement flap may be used. Healing by secondary intention has the disadvantage of lengthening the patient's intra-hospital stay, while the scrotal advancement flap can cause tension sutures responsible for subsequent necrosis. For extensive substance losses, semi-thick mesh skin grafts, free or pediculated fasciocutaneous flaps taken from the anterior part of the abdomen, inguinal region and thigh may be used. At this level, we distinguish the superomedial thigh, inguinal, pudendal and anterolateral thigh fasciocutaneous flaps. In addition to these fasciocutaneous flaps, musculocutaneous flaps may be used. The latter are little used because they provide a thick skin, creating a moist environment that is not favorable to spermatogenesis and promotes maceration, infection [22]. At the end of the reconstruction, the most frequent complications encountered are necrosis of the flap, infection, retractile scars[14].
Table 1: Wound closure option for scrotal reconstruction after debridement
|
Method of skin reconstruction |
indications |
comments |
|
Delayed Primary closure |
Losses of substances limited to the scrotum and constituting less than 25% of the scrotal surface
|
|
|
Healing by secondary intention |
Small losses of substances limited to the scrotum |
|
|
Scrotal advancement flap |
losses of substances limited to the scrotum, less than 50% of the scrotal surface |
|
|
Skin graft · thin · split-thickness |
Extended substance losses, exceeding the scrotal region |
|
|
Flap · fasciocutaneous - Free - pedicle
· Musculocutaneous (adductor minimus, gracilis, and rectus abdominis muscles) |
Large losses of scrotal and perineal substances |
|
|
Large losses of scrotal and perineal substances |
Benefits similar to Fasciocutaneous flaps, but bring excess tissue creating a moist local environment that is favorable for spermatogenesis |
|
|
|
|
*VAC: vacuum-assisted closure
Fournier's gangrene is a medical and surgical emergency. The diagnosis is essentially clinical, helped by imaging and biology. The often-atypical presentation of the disease coupled with high morbidity and mortality requires an urgent diagnosis followed by the implementation of resuscitation measures and aggressive surgical debridement. Tissue reconstruction is the next step in patient management; the knowledge of anatomy, the proper choice of reconstruction method at the appropriate time strongly influence the success of this phase.
LIST OF ABBREVIATIONS
|
°C |
Celsius degree |
|
BPM |
Beat per minute |
|
CT |
Computed Tomography |
|
CRP: |
C reactive protein |
|
DLH |
Douala Laquintinie Hospital |
|
HIV |
Human Immunodeficiency Virus |
|
LRINEC |
Laboratory Risk Indicator for Necrotizing Fasciitis |
The authors would like to thank all the clinicians and staff of the Douala Laquintinie Hospital (DLH) for the care of the patient.
Statement of Ethics
The authors have no ethical conflicts to disclose
Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Any identifying material has been removed, including the patient's name, date of entry, face or any distinctive features on the pictures taken.
Disclosure Statement
The authors have no conflicts of interest to declare
Funding Sources
The authors received no financial support for the research, authorship, and/or publication of this article
Availability of data and material
'Not applicable' in this section
Authors 'contributions
Nwaha and Tchuenkam, contributed in design of the study and writing of the manuscript
Sala, Dongmo, Kabko and Angwafo contributed in critical reading
Nwaha, collected the pictures, and obtained the patient’s consent.
All authors have read and approved the final version of the manuscript.
Stevens DL, Bryant AE. Necrotizing Soft-Tissue Infections. N Engl J Med. 2017 Dec 7;377(23):2253-65. PMid:29211672
View Article PubMed/NCBISarkis P, Farran F, Khoury R, Kamel G, Nemr E, Biajini J, et al. [Fournier's gangrene: a review of the recent literature]. Prog Urol. 2009 Feb;19(2):75-84. PMid:19168009
View Article PubMed/NCBIVoelzke BB, Hagedorn JC. Presentation and Diagnosis of Fournier Gangrene. Urology. 2018 Apr;114:8-13. PMid:29146218
View Article PubMed/NCBIPerkins TA, Bieniek JM, Sumfest JM. Solitary Candida albicans Infection Causing Fournier Gangrene and Review of Fungal Etiologies. Rev Urol. 2014;16(2):95-8.
Fournier Gangrene: Practice Essentials, Background, Anatomy. 2018 Jun 6 [cited 2018 Jun 7]; Available from:
View ArticleFournier JA. Jean-Alfred Fournier 1832-1914. Gangrène foudroyante de la verge (overwhelming gangrene). Sem Med 1883. Dis Colon Rectum. 1988 Dec;31(12):984-8.
View ArticleSchaeffer AJ, Matulewicz RS, Klumpp DJ. Infections of the Urinary Tract. Campbell-Walsh Urol Elev Ed [Internet]. 2016 [cited 2018 Jun 18]; Available from:
View ArticleEke N. Fournier's gangrene: a review of 1726 cases. Br J Surg. 2000 Jun;87(6):718-28. PMid:10848848
View Article PubMed/NCBIVick R, Carson CC. Fournier's disease. Urol Clin North Am. 1999 Nov;26(4):841-9. 70224-X
View ArticleYılmazlar T, Işık Ö, Öztürk E, Özer A, Gülcü B, Ercan İ. Fournier's gangrene: review of 120 patients and predictors of mortality. Ulus Travma Ve Acil Cerrahi Derg Turk J Trauma Emerg Surg TJTES. 2014 Sep;20(5):333-7. PMid:25541844
View Article PubMed/NCBINorton KS, Johnson LW, Perry T, Perry KH, Sehon JK, Zibari GB. Management of Fournier's gangrene: an eleven year retrospective analysis of early recognition, diagnosis, and treatment. Am Surg. 2002 Aug;68(8):709-13.
Eskitaşcıoğlu T, Özyazgan I, Coruh A, Günay GK, Altıparmak M, Yontar Y, et al. Experience of 80 cases with Fournier's gangrene and "trauma" as a trigger factor in the etiopathogenesis. Ulus Travma Ve Acil Cerrahi Derg Turk J Trauma Emerg Surg TJTES. 2014 Jul;20(4):265-74. PMid:25135021
View Article PubMed/NCBIGoh T, Goh LG, Ang CH, Wong CH. Early diagnosis of necrotizing fasciitis. Br J Surg. 2014 Jan;101(1):e119-125. PMid:24338771
View Article PubMed/NCBIKarian LS, Chung SY, Lee ES. Reconstruction of Defects After Fournier Gangrene: A Systematic Review. Eplasty. 2015;15:e18.
Grzybowski A. A short history of Fournier gangrene. Arch Dermatol. 2009 Feb;145(2):182. PMid:19221264
View Article PubMed/NCBILevenson RB, Singh AK, Novelline RA. Fournier gangrene: role of imaging. Radiogr Rev Publ Radiol Soc N Am Inc. 2008 Apr;28(2):519-28. PMid:18349455
View Article PubMed/NCBIWong C-H, Khin L-W, Heng K-S, Tan K-C, Low C-O. The LRINEC (Laboratory Risk Indicator for Necrotizing Fasciitis) score: A tool for distinguishing necrotizing fasciitis from other soft tissue infections*: Crit Care Med. 2004 Jul;32(7):1535-41. PMid:15241098
View Article PubMed/NCBIKincius M, Telksnys T, Trumbeckas D, Jievaltas M, Milonas D. Evaluation of LRINEC Scale Feasibility for Predicting Outcomes of Fournier Gangrene. Surg Infect. 2016 Mar 29;17(4):448-53. PMid:27023717
View Article PubMed/NCBIProfessionals S-O. Urological Infections [Internet]. Uroweb. [cited 2018 Jun 18]. Available from:
View ArticleGangrène de Fournier : prise en charge chirurgicale | Urofrance [Internet]. [cited 2018 Jun 18]. Available from:
View ArticleSingh A, Ahmed K, Aydin A, Khan MS, Dasgupta P. Fournier's gangrene. A clinical review. Arch Ital Urol E Androl. 2016 Oct 5;88(3):157. PMid:27711086
View Article PubMed/NCBIMaguina P, Paulius KL, Kale S, Kalimuthu R. Medial Thigh Fasciocutaneous Flaps for Reconstruction of the Scrotum following Fournier Gangrene: Plast Reconstr Surg. 2010 Jan;125(1):28e-30e. PMid:20048591
View Article PubMed/NCBI