NGOY BULAYA Emmanuel
Telephone: +243814034507; WhatsApp: +243971815256 ;
Email: ngoybulaya@yahoo.fr
© 2019 Sift Desk Journals. All Rights Reserved
VOLUME: 5 ISSUE: 4
Page No: 172-181
NGOY BULAYA Emmanuel
Telephone: +243814034507; WhatsApp: +243971815256 ;
Email: ngoybulaya@yahoo.fr
NGOY BULAYA Emmanuel1*, MALAMBA WA MALAMBA Sylvain2, MULUNGULUNGU N. HO. Ali3, and LUBOYA NUMBI Oscar1, 4.
1*Nutrition Unit, School of Public Health, University of Lubumbashi, DR Congo.
2Nutrition Officer, UNICEF, Lubumbashi, DR Congo;
3Biochestry department, Sciences Faculty, University of Lubumbashi, DRCongo.
1, 4Higher Institute of the Medical Techniques of Lubumbashi, DR Congo.
N. B. EMMANUEL, NUTRITIONAL VALUE OF MASO31 RECIPE AND COMPLEMENTARY FEEDING ACCORDING TO THE WHO RECOMMENDATIONS IN KATANGA, DR CONGO(2020)Journal of Food Science & Technology 5(4) pp:172-181
Inappropriate complementary feeding is among the main causes of malnutrition worldwide. However, optimal complementary feeding is an effective child survival strategy ranked among the top life-saving interventions for children under 5 years. WHO and UNICEF underline the use of available food locally produced for children less than 2 years as a significant strategy to ensure the optimal complementary feeding. Maize-Soy blend in 3/1 proportion (MASO31) is consumed as complementary food in Katanga. Nevertheless, its nutritional value isn’t known nor its adequacy as additional food. This study aimed to evaluate the nutritional value of MASO31 content according to the WHO recommendations on complementary feeding.
Two samples of MASO31 formulas were taken of two different preparations, for biochemical analysis nutrients data (energy, protein, Fe, Ca, P, Zn) in the Research and Agro Alimentary Analysis Center (CRAA) of Lubumbashi. The biochemical methods used were specific to analyze each nutrient data in MASO31 such as conversion factors and KJELDHAL. Comparative analysis of «MASO31» content was done using the WHO Complementary Feeding Recommendations as gold standard.
Energy and nutrients content of 100g of «MASO31» were higher than the WHO Recommendations for complementary feeding period in daily need. But, calcium and phosphorus content was lower than the recommendations and needed improvements. The number of times that was proposed by ACANUDE NGO for «MASO31» to be fed is similar to the WHO recommendations on meal frequency in complementary feeding.
MASO31 may be recommended in complementary feeding in DRC but calcium and phosphorus content should be enriched.
Key words: Adequate complementary food, Complementary feeding, Democratic Republic of the Congo, Local complementary food and Nutritional value.
Highlights
1.1. CONTEXT AND BACKGROUND
The World Health Organization (WHO) has recommended, since 1998, that children should be exclusively breastfed for the first six months, followed by continued breastfeeding (BF) with complementary feeding (CF) from 6 months up to two years or over two years (Motee A, Jeewon R. 2014; Liatard M. et al. 2014 ; Rao S. 2011; Issaka A.I.et al. 2014 and Issaka A.I. et al. 2015) in order to achieve optimal growth, development and child health. During this period, children may be affected by acute malnutrition, which may lead to mortality or to stunting, if they consume insufficient quantities and poor quality of additional food over a long-time, even if they received optimal breastfeeding (Rao S. 2011; Issaka A.I.et al. 2014 and Issaka A.I. et al. 2015). In spite of the WHO Infant and Young Child Feeding (IYCF) recommendations, malnutrition is always one of the main public health challenges of the 21st century, particularly in developing countries (Butha Z.A. and Salam R.A. 2012; Tigist Kassa et al. 2016; Semahegn A. 2014; Lassi ZS et al. 2013). In 2016, wasting affected almost 51.5 million children less than 5 years worldwide and was attributable cause of 12.6% of 6.9 million deaths with more than one third related to inadequate CF (Butha Z.A. and Salam R.A. 2012; Semahegn A. 2014; Lassi ZS et al. 2013; James P et al. 2016; Langendorf C. et al. 2014; and Hong Zhou PhD1 et al. 2012). Nineteen million of them were severely affected and at higher death risk with a large majority from sub-Saharan Africa countries including Democratic Republic of the Congo (DRC). Democratic Republic of the Congo (DRC) is one of 34 developing countries where malnutrition is the major problem of public health. Around one out of two children younger than 5 years was stunted, more than 6 million children under 5 years were wasted and 1.9 million of severe acute malnutrition cases were estimated in 2017. Around 600000 children less than 5 years die every year from consequences of malnutrition (UNICEF RDC 2014). Food insecure people were approximately 80 million in 2015 and 108 million in 2016 in the world (ENN, NUTRITION EXCHANGE 2017). Seven out of ten households were food insecure in 2016 within DRC (PAM and INS-DRC 2016).
1.2. STATEMENT OF PROBLEM
Inadequate complementary feeding (CF) is among the principal causes of malnutrition worldwide while the optimal complementary feeding was shown to be an effective child survival strategy ranked among the top life-saving interventions for children under 5 years. The determinants of inappropriate CF are low energy and nutrient quality of the additional food not counting others environmental variables concerned (Dewey KG and Mayers DR 2011; Christine P. Stewart et al. 2013; Saaka M et al. 2015). Alone, optimal CF could prevent almost 6 to 20% of under-five mortality in developing countries (Fahmida U et al. 2015; Haile D et al. 2015; Tiwari Rina et al. 2014). In DRC, the DHS-2013-2014 reported that the CF practices were poorly observed and a high prevalence of malnutrition was reported (UNICEF RDC 2014 and RDC MNSP MNP MNA 2014). The World Food Program (WFP) and DRC-Plan Ministry (2016) found a higher prevalence of food insecurity than in 2013-2014 (PAM and INS-DRC 2016). However, there is limited evidence and knowledge on adequacy of additional foods locally produced and consumed. The Non-Governmental Organization of Development (NGOD) ACANUDE had developed a local food mixture based on a maize-soy blend mixture in 3/1 proportions, named «MASO31». It is used in some DRC-provinces in CF, but its energy and nutrients content is unknown.
1.3. RATIONALE
World Health Organization and UNICEF underline the use of locally available food products for children less than 2 years as a significant strategy to ensure optimal complementary feeding for growth, development, and optimal wellbeing of children in the first crucial 1000 days (8 and 19). Knowledge on nutritional value of «MASO31» formulas used as complementary foods in DRC will serve health authorities’ planners to better orient; to better plan the nutritional program and the mothers to use accessible and available adequate additional food for their children. This will help to prevent malnutrition and indirectly to contribute achieving the second sustainable development goal “End hunger, achieving food security and improved nutrition and sustainable agriculture”. It will be possible to improve CF practices with available locally produced food mixture, «MASO31», as recommended by WHO and UNICEF. mm»MASO31» is geographically and financially accessible, socio-culturally accepted and locally available solutions to the rural people in DRC, allowing the reduction of malnutrition rate. The results of the present study will contribute a new piece of evidence base for other researchers in DRC.
1.4. OBJECTIVE
This study aimed to evaluate the nutritional value of «MASO31» content according to the complementary feeding WHO recommendations.
2.1. Study area
MAO31 formula is a maize-soya blend mixture used in complementary feeding, prepared by ACANUDE NGOD and consumed in the entire DRC especially in Ex Katanga province where mining remains the principal occupation of most people. A minority of people have agriculture as the main occupation while few of them are involved in trading. The principal staple foods include cereals (maize, rice), tubers, legumes (beans), nuts (peanuts), vegetables and many animal and vegetable imported foods.
2.2. Design, sampling, techniques method and target population of MASO31
In a fundamental study, a biochemical method was used to determine the nutritional value of 100 grams of MASO31 in terms of energy, proteins and micronutrients. Two samples of Maize-Soy blend, MASO31 formula, were taken from two different preparations for biochemical analysis. Energy, and nutrients (protein, Fe, Ca, P, Zn,) were analyzed in the Research and Agro-alimentary Analysis Center (CRAA) of Lubumbashi (ILUNGA NDALA W 2014). Conversion factors, Kjeldhal, non-azoted extractive and spectrometry of plasma inductive coupling emission were the methods used for analyses.
The moisture content of MASO31 was determined by the loss of weight due at the beginning of water by evaporation following the rise in the temperature. The procedure was to introduce 5g of MASO31’ mass in a dried and tared capsule. Then, to place the capsule in the drying oven (HERAUS) at 105°C for 24 hours. The capsule was withdrawn from the drying oven and was coupled with the desiccator during 30 minutes and then weighed. After another 12 hours in the drying oven, the capsule was weighed until constant weight.
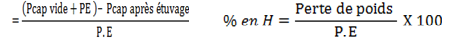
Legend: Pcap vide = weight of the empty capsule. Pcap après étuvage = weight of the capsule after heating. Pcap vide + Pcap après étuvage = Perte de poids = loss of weight (moisture). PE = Weight of the test specimen.
The KJELDHAL method was used to determine MASO31 protein content. Proteins were dosed indistinctly starting from total nitrogen. The method consisted in mineralizing samples in the concentrated sulphuric acid with sodium or potassium sulphate, copper sulfate and mercury chloride, such that all nitrogen, except for the nitrate nitrogen, was transformed into ammoniac. This last product was then distilled in alkaline mediums and was collected by an acid solution titrated by a base. The following materials were used : analytical METTLER device of distillation balances, pipettes and washing bottles and drying Kjeldhal balloon. The concentrated sulphuric acid, copper sulfate, mercury chloride (Hg Cl), sodium sulphate and soda 10 N (soda detergent), hydrochloric acid (HCl 0,1N), soda (0,1N), mixed indicator: red of bromothymol (RB) and phenolphthalein were the reagents to achieve the protein analysis content in MASO31. The process was the mineralization of 2g of MASO31-distillation-titration and expression of the results.
The MASO31 fat content was obtained using the Soxhlet method which consisted to extract the fat content by an organic solvent with the heat effect by the Soxhlet apparatus. The process was that 5g of MASO31 was carefully introduced into a cartridge in cellulose. Then the cartridge was introduced into the apparatus of Soxhlet and to assemble the device to backward flow, to carry to boiling 100 ml of n-hexane for 8 hours. Quantitatively solvent charged with matters was transferred in a clean, dry balloon container. The solvent was driven out and the balloon was dried with the regulated drying oven at 105C cooled in the desiccator and weighed. The results were expressed by :
![]()
Legend : P.E = weight of specimen test, MG = Fat Mass
The totals carbohydrates content of MASO31 were determined using EXTRACTIVE NOT NITROGEN METHOD. The MASO31 total carbohydrates content was obtained by calculation as follows: % carbohydrates total = 100 - (Proteins +Lipides + Ashes + Cellulose). The calculation compared to the dry matter.
The energy value (kcal) of MASO31 was calculated using the following conversion factors : 1g of protein = 4Kcal, 1g of carbohydrates = 4Kcal and 1g of lipids = 9Kcal.
The SPECTROMETRY Of PLASMA INDUCTIVE COUPLING (ICP) EMISSION method allowed to analyse micronutrients content of MASO31, especially Cu, Fe, Ça, P, Mn, Zn. Firstly, setting in solution by mineralisation by way dries in eliminating the organic matter and silica from the samples, this method makes it possible to put in solution, for their proportioning, a great number of biogenic salts. Procedure: to weigh 0,2g matter in a tube test beforehand washed, dried with the drying oven and tared, to introduce the matter into the test tube more 15 ml of water levels, heated on the plate with the total dissolution of the sample. After cooking, the solution obtained was diluted in a balloon of 100 ml and was supplemented with the water distilled to the feature of gauge; if it has residue one filters the solution. After having adjusted with water distilled with the feature of gauge the solution was homogenized by agitation. Secondly, proportioning of the biogenic salts. The preceding solution was analyzed using a spectrometer VARIAN VISTA (Victoria, Australia), equipped with a detector C CD (To couple To charge Device) allowing the simultaneous determination, with several wavelengths, of all the elements of the periodic classification of the elements except for the gas body. Proportionings were carried out by carrying out a calibration observing the conditions of the analyzed medium: stamp, acidity. The validation of the results rests on the analysis of a reference sample whose content of biogenic salts was known. These witnesses followed the same analytical advance rigorously that the samples and were introduced at a rate of minimum witness for 20 samples. The nutritional value of MASO31 in vitamin A and in Niacin was not analyzed in the laboratory but the Vitamin A and B1 were calculated from the food composition tables of the DRCongo.
Systematic proportional methods allowed us to identify the projected introduction time of MASO31 formula in IYCF and to examine the daily MASO31 consumption in terms of energy, proteins and micronutrients considering the meal frequency recommended by ACANUDE. Comparative analysis of MASO31 nutritional value was done using the WHO Recommendations for complementary feeding as gold standard. The target population of present study was children from 6 to 23 months old.
2.3. Adequacy of complementary food
The recommended energy and frequency of the adequate Complementary Food in the developing countries are: 200 kcal 2 to 3 times per day for infants 6-8 months of age; 300 kcal 3 to 4 times per day at 9-11 months of age and 550 kcal 3-4 times per day at 12-23 months of age (Mohammad Rocky Khan Chowdhury et al. 2016; Beyene M. et al. 2015; Ghosh S et al. 2014; Dennis J. Matanda et al. 2014; Malhotra N 2012 and Nancy F Butte et al 2000). The recommended daily quantities of nutrients in the adequate Complementary Food are: 0.9 gr of proteins/100kcal, 1mg of iron/100kcal, 63 mg of calcium/100kcal and 0.6 mg of zinc/100kcal (Nancy F Butte et al 2000; Kathryn G. Dewey and Kenneth H. Brown 2003).
2.4. MASO 31 formula description
MASO31 is a complementary food formula developed by ACANUDE NGOD in Tanganyika Province in 2013, DRC. The first aim of ACANUDE was to provide and present an additional food mixture locally produced which would be available, geographically, and financially accessible and socio-culturally accepted in the rural areas. Secondly, ACANUDE NGOD aimed to provide one complementary food formula with a high biological value able to meet the nutritional requirements of the children from 6 to 23 months old and for pregnant & nursing women. Children consume MASO31 in gruel form (mush form, mess form, porridge form, and puree form). The daily dosage is determined in the table I. In the empirical study conducted, MASO31 formula was digestible and acceptable in most children. That is why a randomized controlled trials study will be undertaken to assess effectiveness of MASO31 formula (nutritional impact on the nutritional status).
2.5. Composition of the MASO 31 in ingredients predicted by ACANUDE NGOD
The MASO31 composition-ingredients converted into local measurements, in considering a standard measurement, comprises 3 measures of the maize flour, 1 measure of soya flour, ½ measure of sugar, ½ measure of palm oil and 1/10 measure of cooking salt. To the whole mixture of maize-soya blend, one adds the flour of germinated dried maize representing a tenth of the whole mixture quantity. This is to make the MASO31 digestive. Before mixing ingredients, soya grain is roasted and ground in flour while the maize flour is too roasted until to obtain the yellow coloration enhancing energetic balance and taking away nutrient antagonists like phytic acid and polyphenols. All components of the MASO31 formula are always consumed in the study area. Below table I, the daily dose and the daily frequency of MASO31 per age bracket of children, pregnant and nursing women are presented as recommended by ACANUDE NGOD.
2.6. Data quality control analysis and potential biases mitigation
In an effort to have quality results, two different samples of Maize and Soya blend “MASO31” formulas were taken from two different preparation batches aiming to ensure the reliability and validity of samples analyzed in the CRAA which is recognized as regards food agro analysis.
2.7. Data analyses
The comparative analyses of MASO31 content with the CF WHO Recommendations were done. Details in table 1.
2.8. Ethics consideration
The permission to carry out this study was sought from Health Province authorities and the study protocol was approved by the ethical committee of the University of Lubumbashi in DRC (N° UNILU/CEM/201/2020 eth_med@yahoo.fr in Mach 14, 2020) in order to guarantee the respect of the person, the benevolence and the equitable & honest distribution of the risks & benefit of the study. The MASO31 formula is prepared in mixing the foods currently eaten by the people in DRC. So MASO31 is not constrained and could not provide any disadvantage to children.
Table 1: Daily dose of the MASO31 per age bracket and daily meal frequency recommended by ACANUDE
|
Age bracket in months |
Daily dose of the MASO31 expressed in international measure |
Daily dose of the MASO31 expressed in local measure |
Daily MASO31 frequency consumption |
|
6 to 11 |
100 to 150 g |
½ to ¾ ordinary household cup |
1 to 2 times |
|
12 to 23 |
150 to 200 g |
¾ to 1 ordinary household cup |
2 to 3 times |
|
24 to 35 |
200 to 250 g |
1 to .25 ordinary household cup |
3 to 4 times |
|
36 to 47 |
250 to 300 g |
1.25 to 1.5 ordinary household cup |
4 times |
|
48 to 59 |
300 to 350 g |
1.5 to 1.75 ordinary household cup |
4 times |
|
Pregnant wife |
350 to 400 g |
1.75 to 2 ordinary household cup |
2 times |
|
Nursing wife |
400 to 500 g |
2 to 2.5 ordinary household cup |
3 times |
The agro alimentary Bulletin of the results of analyses realized by the Research and Agro alimentary Analysis Center is presented below in Table 2.
3.1. Nutritional value of MASO31 determined by CRAA
Table 2, shows the energy, macronutrients and micronutrients content of the MASO31 formulas.
3.2. The introduction time of MASO31 formulas to the children
Table I shows the daily dose of the MASO 31 per age bracket recommended by ACANUDE according to the daily nutritional needs of children from 6 to 23 months old.
3.3. The daily MASO31 doses per age bracket recommended by ACANUDE
Regarding the finding in table 1, children 6-11 months old must consume 150 g of MASO31 one to two times daily while those 12-23 months old can consume 200 g of MASO31 two to three times daily.
3.4. Comparative analysis of the daily MASO31 energy contribution with complementary feeding World Health Organzation Recommendations
The finding in table 3 shows that MASO 31 largely covers complementary WHO Recommendations in term of daily energy need and in term of frequency.
3.5. Comparative analysis of daily MASO31 proteins and micronutrients contribution recommended by NGOD ACANUDE with the complementary feeding WHO recommendations
The proteins, iron and zinc content from the recommended daily amount of MASO31 were more than the WHO recommendation but, calcium and phosphorus content were lower as shown in table 4.
Table 2. The nutritional value of 100 grams of MASO31 in term of energy, macronutrients and micronutrients (ILUNGA NDALA W. 2014).
|
Nutrients Analyzed |
Sample 1 |
Sample 2 |
|
Moisture (g) |
8 |
8 |
|
Energy (kcal) |
409 |
410 |
|
Lipides(g) |
13 |
14 |
|
Protéines(g) |
13 |
11 |
|
Glucides(g) |
60 |
60 |
|
Cellulose (g) |
1 |
1 |
|
Cu (mg) |
5.2 |
0 |
|
Fe (mg) |
18 |
16 |
|
Ca (mg) |
201 |
201 |
|
P (mg) |
159 |
159 |
|
Mn (mg) |
2 |
2 |
|
Zn (mg) |
7 |
7 |
|
Pl (mg) |
1.6 |
1.6 |
|
Vit. A (mg) |
28 |
28 |
|
Vit. B1 (mg) |
0.24 |
0.24 |
Table 3. Comparative analysis of the daily MASO31 energy, proteins & micronutrients and his daily frequency recommended by ACANUDE wtith complementary feeding WHO Recommendations (Rao S et al. 2011; Fahmida U et al. 2015).
|
Age bracket in months |
Daily Contribution of the MASO 31 (in Kcal) per child |
Frequency MASO31 |
Daily Contribution of CF / WHO Recommended in Kcal per child |
Frequency of CF / WHO Recommended |
|
8 to 9 |
615 |
1 to 2times |
200 |
2 to 3 |
|
9 to 11 |
615 |
1 to 2times |
300 |
3 to 4 |
|
12 à 23 |
820 |
2 to 3 times |
550 |
3 to 4 |
Table 4. Comparative analysis of daily MASO31 dose quantity of proteins and micro nutrients contribution with Daily Standards WHO Recommended Contributions in proteins and micronutrients by 100Kcal (Fahmida U et al. 2015).
|
Analyzed nutrients |
Sample 1 MASO 31 |
Sample 2 MASO 31 |
Standards WHO Recommandations |
|
Proteins(g/100 Kcal) |
3,24 |
2,75 |
0,9 |
|
Fe (mg/100 Kcal) |
4,5 |
4,0 |
1,0 |
|
Ca (mg/100 Kcal) |
50,25 |
50,25 |
63,0 |
|
P (mg/100 Kcal) |
40,0 |
40,0 |
63,0 |
|
Zn (mg/100 Kcal) |
1,75 |
1,75 |
0,6 |
|
Niacin (mg) |
NA |
NA |
0,9 |
Exploring and assessing MASO31 energy, proteins and minerals content, the table II shows that MASO31 gives the laboratory result analysis and shows that it contained all required nutrients. Concerning the introduction time of MASO31 formulas in the Complementary Feeding, according to the ACANUDE documentation on MASO31 development, MASO31 may be introduced by the 6th month of age. The minimum meal frequency and the minimum dietary diversity in terms of energy, proteins and micronutrients recommended for MASO31 formulas, as shown in tables 1, 3 and 4 are similar to the WHO minimum meal frequency because the MASO31 can be fed to the children two to four times per day. In table 3 we observe that the expected MASO31 energy content was higher than the WHO Recommendations. Then in table 4, MASO31 covers entirely the standards WHO recommends for energy, proteins, in iron and in zinc, but only 63% and 80% of the standards WHO recommends respectively for phosphorus and calcium. The niacin content is not known because no vitamin analyses were done. A similar cereal-legume blend showed improved growth in children in Ghana (Madoka Inoue and Colin W. Binns 2014). Our previous research about complementary feeding habits in DRC, indicated that most mothers usually give maize-soya based-recipes because maize and soy are available, locally produced and not constrained. Among many constraints to improve child nutrition through quality CF, there is acceptability, which is important one when the foods are imported or of external origin (Mohamed Ag Ayoya et al. 2010). In Southeast Asian Countries, complementary feeding is rice-based and contains low amounts of animal source food partly because of lack of knowledge about nutrient-rich food because of economic constraints (Fahmida U and Preedy VR 2012). These cereal-based diets have high anti-nutrients content such as polyphenols and phytic acid that could compromise iron and zinc absorption (Gbson RS, Baley KB, Gibbs M et al. 2010). It was shown that plant-based complementary foods used in low in-come countries are associated with micronutrient deficiencies, especially of iron, zinc and calcium (Santika O et al. 2009; Enderson VP, Cornwall J, Jack S et al. 2008; Gibson RS, Ferguson EL and Lehrfeld J. 1998). As stated previously, maize and soy in MASO31 are toasted before their mixing to remove phytate and polyphenols, allowing iron and zinc bioavailability, avoiding micronutrient deficiencies. Caterpillars ‘powder is recommended to be added for improving phosphorus and calcium content of MASO31. Willett et al, in the EAT-Lancet Commission on Health Diet from Sustainable Food System, emphasized that “a diet rich in plant-based foods and with fewer animal source food confers both improved health and environmental benefits” (Walter Willett MD, Johan Rockstrom et al. 2017). In Myanmar, the 12-23 months old children diet remained inadequate in niacin, folate, thiamin, Fe, Zn, Ca and vitamin B6 and an acceptable set of complementary foods recipes were developed to improve the dietary practices of Myanmar children in using locally available foods. An alternative intervention was the fortification with the locally available vegetables and nutrient-dense foods that would fill the nutrient gaps (Lwin Mar Hlaing et al. 2016). This corroborates the “MASO31” recipe component and enrichment with caterpillars. All ingredients of MASO31 are locally available, non-constrained in our study area.
LIMITS OF RESEARCH
Present research did not assess the availability of MASO31 in the study area. The physical, geographical, socio-cultural and financial accessibility were not assessed in this study. According to the financial limitation, our research focused on evaluating introduction time, minimum meal frequency, energy, protein and micronutrient content of the MASO31 only. We did not assess the nutritional impact of MASO31 in the growth of children.
All comparison analysis of MASO31 content in energy, proteins and micronutrients with the complementary feeding WHO Recommendations highlight MASO31 recipe as an adequate complementary food in DRC. Improvements of MASO31 in calcium and phosphorus by adding local caterpillars powder are recommended. A Randomized Controlled trial is needed to determine the effects of MAO31 on infant’s growth during complementary feeding period.
We would like to thank Professor Salome Kruger from the Centre of Excellence for Nutrition N-W University, Potchefstroom, South Africa for her help to review this paper.
Any form of outside grant was obtained to support this study.
Beyene M. et al. Dietary diversity, meal frequency and associated factors among infant and young children in Northwest Ethiopia: a cross- sectional study, BMC Public Health2015 15:1007 DOI: 10.1186/s12889-015-2333-x PMid:26433689
View Article PubMed/NCBIButha Z.A. and Salam R.A., While poverty and socioeconomic inequity remains an important factor, in many cases, the presence of micronutrient deficiency is a factor of diet quality, Global Nutrition Epidemiology and Trends, Ann Nutr Metab 2012; 61 (suppl 1): 19-27 PMid:23343944
View Article PubMed/NCBIChristine P. Stewart*, Lora Iannotti†, Kathryn G. Dewey*, Kim F. Michaelsen‡ and Adelheid W. Onyango, Contextualizing complementary feeding in a broaderframework for stunting prevention, 2013, WHO, Geneva, Switzerland DOI: 10.1111/mcn.12088 PMid:24074316
View Article PubMed/NCBIDennis J. Matanda , Maurice B. Mittelmark, Dorcus Mbithe D. Kigaru , Breast-,complementary and bottle-feeding practices in Kenya: stagnant trends were experienced from 1998 to 2009, 2014, Elsevier, Available online at www.sciencedirect .com Science Direct PMid:25026918
View Article PubMed/NCBIDewey KG, Mayers DR: Early child growth: how do nutrition and infection interact? Matern Child Nutr 2011; 7: 129-142. PMid:21929641
View Article PubMed/NCBIEnderson VP, Cornwall J, Jack S et al. (2008) Intake for no-breastmilk foods for stunted toddlersliving in power urban villages of Phnom Penh, Cambodia are inadequate. Matern Child Nutr 4, 146 - 159. PMid:18336647
View Article PubMed/NCBIENN, NUTRITION EXCHANGE Équateur: Stratégies de lutte contre l'obésité; Afrique de l'Ouest : Plaidoyer pour la nutrition au sein de la société civile; Népal : Les voix du terrain, ISSN 2050-3733, Juillet 2017 - Numéro 8
Fahmida U and Preedy VR (2012) Food-based complementary feeding and its impact on growth: Southeast Asian Perspectives:Handbook of Growth and Growth monitoring in health and disease, New York: Springer.
View ArticleFahmida U, Kolopaking R, Santika O, Sriani S, Umar J, Htet MK, et al. Effectiveness in improving knowledge , practices , and intakes of " key problem nutrients " of a complementary feeding intervention developed by using linear programming : experience in Lombok , Indonesia 1 - 3. 2015; Downloaded from ajcn.nutrition.org at Congo, the Democratic Republic of the: ASNA Sponsored on October 4, 2016 PMid:25733629
View Article PubMed/NCBIGbson RS, Baley KB, Gibbs M et al. (2010) A review of phytate, zinc, iron and calcium concentration in plants-based complementary foods used in low-income countries and implications for bioavallability. Food & Nutrition Bulletin 36, Suppl. 2, 134 - 146. PMid:20715598
View Article PubMed/NCBIGhosh S, Tano-debrah K, Aaron GJ, Otoo G, Strutt N, Bomfeh K, et al. Improving complementary feeding in Ghana : reaching the vulnerable through innovative business - the case of KOKO Plus. Ann. N.Y. Acad. Sci. ISSN 0077-89232014;1331:76-89. PMid:25514865
View Article PubMed/NCBIGibson RS, Ferguson EL and Lehrfeld J (1998) Complementary food for infant feeding in developing countries: their nutrients adequacy and improvement. Eur J Clin Nutr52, 764 - 770. PMid:9805226
View Article PubMed/NCBIHaile D, Belachew T, Berhanu G, Setegn T and Biadgilign S, Complementary feeding practices and associated factors among HIV positive mothers in Southern Ethiopia Haile et al. Journal of Health, Population and Nutrition (2015) 34:5 DOI 10.1186/s41043-015-0006-0 PMid:26825277
View Article PubMed/NCBIHong Zhou PhD1, Xiao-Li Wang PhD1, Fang Ye BSc1, Xiaopei Lily Zeng BSc2, Yan Wang DrPH1, Relationship between child feeding practices and malnutrition in 7 remote and poor counties, P R China, Asia Pac J ClinNutr 2012;21 (2):234-240
James P, Sadler K, Wondafrash M, Argaw A, Luo H, Geleta B, et al. (2016) Children with Moderate Acute Malnutrition with No Access to Supplementary Feeding Programmes Experience High Rates of Deterioration and No Improvement: Results from a Prospective Cohort Study in Rural Ethiopia. PLoSONE 11(4): e0153530. doi:10.1371/ journal.pone.0153530 Editor: Sergio Pellis, University of Lethbridge, CANADA PMid:27100177
View Article PubMed/NCBIILUNGA NDALA W., Bulletin des résultats d'Analyses de l'aliment de sevrage MASO 31 n° 020/2014, Centre de Recherche Agro-Alimentaire, C.R.A.A.,2014 Lubumbashi, DRC,.
Issaka A.I.et al., Determinants of inadequate complementary feeding practices among children aged 6-23 months in Ghana, May 2014, Public Health Nutrition: 18(4), 669-678 doi:10.1017/S1368980014000834 PMid:24844532
View Article PubMed/NCBIIssaka A.I. et al, Practices among children aged 6-23 months in four Anglophone West African countries, original article, 2015, DI: 10, 1111/mcn.12194
Kathryn G. Dewey and Kenneth H. Brown, Update on technical issues concerning complementary feeding of young children in developing countries and implications for intervention programs, Food and nutrition bulletin, vol.24, n° 1 @ 2003, The United Nations University PMid:12664525
View Article PubMed/NCBILangendorf C, Roederer T, de Pee S, Brown D, Doyon S, et al. (2014) Preventing Acute Malnutrition among Young Children in Crises: A Prospective Intervention Study in Niger. PLoS Med 11(9): e1001714. doi:10.1371/journal.pmed.1001714 PMid:25180584
View Article PubMed/NCBILassi ZS, Das JK, Zahid G, Imdad A, Bhutta ZA. Impact of education and provision of complementary feeding on growth and morbidity in children less than 2 years of age in developing countries : a systematic review. BMC Public Health [Internet]. 2013;13(Suppl3):S13. PMid:24564534
View Article PubMed/NCBILiatard M, Champagne-ardenne CCI, Ardenne C, Bsdd L, Class I. Fiches techniques Alimentation du nourrisson et du jeune enfant,MINISANTE, PRONANUT, 2014;1-2.
Lwin Mar Hlaing1,2*, Umi Fahmida2, Min Kyaw Htet3, Budi Utomo4, Agus Firmansyah5 and Elaine L. Ferguson6 Local food-based complementary feeding recommendations developed by the linear programming approach to improve the intake of problem nutrients among 12-23-month-old Myanmar children, British Journal of Nutrition (2016),116(S1), S16-S26 PMid:26696232
View Article PubMed/NCBIMadoka Inoue and Colin W. Binns, Introducing Solid Foods to Infants in the AsiaPacific Region, nutrients, 2014 ISSN 2072-6643 PMid:24399099
View Article PubMed/NCBIMalhotra N, Inadequate feeding of infant and young children in India: lack of nutritional information or food affordability?, 2012, India, Public Health Nutrition: 16(10), 1723-1731 doi: 10.1017/S1368980012004065 PMid:22939461
View Article PubMed/NCBIMohamed Ag Ayoya, Joseph Kodio, Akory Ag Iknane and Roger Sodjinou, Nutritional value of locally produced foods and potential for developing age- appropriate complementary foods for children under 2 years of age in Mali, Food and Nutrition Bulletin, vol. 31, no. 3 © 2010, The United Nations University. PMid:20973460
View Article PubMed/NCBIMohammad Rocky Khan Chowdhury1, Md. Shafiur Rahman1,2 and Md. Mobarak Hossain Khan3,4*, Levels and determinants of complementary feeding based on meal frequency among children of 6 to 23 months in Bangladesh, BMC Public Health BMC series - open, inclusive and trusted 2016 16:944 DOI: 10.1186/s12889 -016-3607-7 PMid:27604631
View Article PubMed/NCBIMotee A, Jeewon R. Importance of Exclusive Breast Feeding and Complementary Feeding Among Infants, Current Research in Nutrition and Food Science Vol. 2 (2), 56-72 (2014)
View ArticleNancy F Butte et al., Energy requirements derived from total energy expenditure and energy deposition during the first 2 years of life. Am J Clin Nutr 2000; 72:1558-69 PMid:11101486
View Article PubMed/NCBIPAM and INS-DRC, Evaluation approfondie de la sécurité alimentaire dans la Province de Haut Katanga, Haut LOMAMI, Lualaba et Tanganyika, Aout 2016, PAM, DRC
Saaka M. Anthony Wemakor, Abdul-Razak Abizari and Paul Aryee, How well do WHO complementary feeding indicators relate to nutritional status of children aged6-23 months in rural Northern Ghana?, BMC Public Health (2015) 15:1157 DOI 10.1186/s12889-015-2494-7 PMid:26596246
View Article PubMed/NCBISantika O, Fahmida U, and Ferguson EL (2009) Development of food-based complementary feeding recommendations for 9 to 11 month-old peri-urbanIndonesian infants using linear programming. J. Nutrition 139, 135 - 141 PMid:19056658
View Article PubMed/NCBISemahegn A, Tesfaye G, Bogale A. Complementary feeding practice of mothers and associated factors in Hiwot Fana specialized hospital, eastern Ethiopia. Pan Afr Med J. 2014;18:1-11. PMid:25419281
View Article PubMed/NCBIRao S, Swathi P, Unnikrishnan B, Hegde a. Study of complementary feeding practices among mothers of children aged six months to two years - A study from coastal south India. Australas Med J [Internet]. 2011;4(5):252-7. PMid:23393516
View Article PubMed/NCBIRDC MNSP MNP MNA, Rapport final EDS - RDC, 2014;2013-4
Tigist Kassa, Berhan Meshesha, Yusuf Haji and Jemal Ebrahim, Appropriate complementary feeding practices and associated factors among mothers of children age 6-23 months in Southern Ethiopia, 2015, BMC Pediatrics, 2016, 16:131 PMid:27542833
View Article PubMed/NCBITiwariRina *, Ausman Lynne M and Kingsley Emwinyore Agho, Determinants ofstunting and severe stunting among under-fives: evidence from the 2011 Nepal Demographic and Health Survey, BMC Pediatrics 2014, 14:239, PMid:25262003
View Article PubMed/NCBIWalter Willett MD, Johan Rockstrom et al. EAT-Lancet Commission on Health Diet from Sustainable Food System, thelancet.com/commission/EAT.
UNICEF RDC, la nutrition chez les enfants de moins de cinq ans en République Démocratique du Congo, NARRATIF COMMUN, UNICEF RDC, 2014 Almeras
